From 619 Drugs to 1: Researchers Uncover Hidden Risk

Introduction: Addiction Risk in Commonly Prescribed Drugs
When you think of medication side effects, your mind probably goes to the warnings listed in commercials. Drowsiness, nausea, dizziness, etc. These are common, often manageable, and generally expected side effects of drugs.
But what about far more profound ones that can alter your behavior, strain your relationships, and impact your life?
A recent study delved into this very issue, analyzing VigiBase®, the World Health Organization’s global pharmacovigilance database, containing over 36 million adverse event reports, to uncover surprising links between everyday medications and the development of behavioral addictions.
The research sought to identify drugs where these life-altering risks are not officially listed, leaving us in the dark. This post will break down the most impactful findings from that detective work.
Takeaway 1: It’s Not Just the Usual Suspects Anymore
For years, the primary link between medication and behavioral addiction centered on a specific class of drugs: dopaminergic antagonists used to treat Parkinson’s disease.
The connection was so well-established that it was considered the main, and for many, the only, example of this phenomenon. This new study dramatically broadens that scope.
By analyzing reports from healthcare professionals worldwide, researchers identified seven classes of drugs associated with behavioral addictions, even though this risk is not officially listed as a side effect for them. These include:
- Antidepressants
- Antipsychotics (specifically, dopamine antagonists)
- Antiepileptics
- Benzodiazepines or related drugs
- Psychostimulants
- Retinoids
- One antidiabetic drug
This finding is significant because it suggests the problem is far more widespread than previously understood. It potentially affects patients being treated for a wide range of common conditions.
Are you a professional looking to stay up-to-date with the latest information on, sex addiction, trauma, and mental health news and research? Or maybe you’re looking for continuing education courses?
Stay up-to-date with all of Dr. Jen’s work through her practice’s newsletter!

Takeaway 2: A Widely Used Antipsychotic Emerged as a Primary Concern
From an initial pool of 619 suspect medications reported at least five times, researchers applied a rigorous filtering process to hunt for the strongest signals. Ultimately, only one drug, Olanzapine, met all of the study’s highest evidence-based criteria.
Olanzapine is a second-generation antipsychotic medication.
The study found that it had the most well-documented cases with strong evidence linking it to behavioral addiction. This evidence included reports where symptoms resolved after:
- The patient stopped taking the drug (a “positive dechallenge”)
- A significant statistical signal in the data
- Support from existing scientific publications
The study’s authors emphasized how their multi-step analysis narrowed the field to this single, compelling candidate:
Our analysis allows to narrow down the search to include only the most thoroughly documented cases… This process culminated in reducing the initial count of 619 suspect to 1: Olanzapine.
While Olanzapine was the only drug to meet every one of the study’s strictest criteria, the researchers noted that other antipsychotics also showed significant warning signs in the data. The specific behavioral addictions most strongly linked to Olanzapine included a range of behaviors such as binge eating, compulsive sexual behavior, compulsive shopping, and gambling disorder.
Takeaway 3: This Hidden Danger Isn’t Listed on the Drugs Official Label
The core purpose of the study was to identify drugs for which behavioral addiction is not listed as a known side effect in the official Summaries of Product Characteristics (SPCs). These are the detailed documents that guide doctors on a drug’s use and risks.
The implication of this is critical: patients and even some doctors may be completely unaware of these potential risks when prescribing or taking these medications.
An individual experiencing a sudden onset of compulsive behavior might not connect it to their prescription, leading to confusion, distress, and delayed intervention. This research underscores the importance of “pharmacovigilance,” the ongoing science of monitoring drug safety after a medication is on the market.
It is a crucial tool for uncovering hidden patterns and rare side effects that may not have appeared in initial clinical trials.
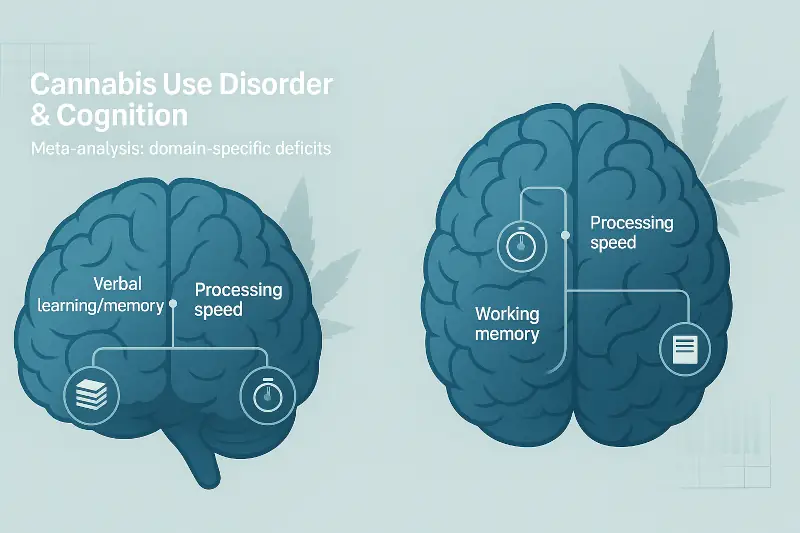
Do you have enough hours for your LPC renewal? Are you in need of continuing education, but bored with the current offerings? Check out Dr. Weeks’ course on Cannabis Use Disorder, and other unique courses on her practice website.
Sexual Addiction Treatment Services has been approved by NBCC as an Approved Continuing Education Provider, ACEP No. 7250. Programs that do not qualify for NBCC credit are clearly identified. Sexual Addiction Treatment Services is solely responsible for all aspects of the programs.
Takeaway 4: The Brain Science is More Complex Than Just Dopamine
Addiction is often explained through the lens of the brain’s reward system, which is heavily driven by the neurotransmitter dopamine.
This is why dopaminergic drugs for Parkinson’s were the first to be linked to behavioral addictions. However, the study’s findings on drugs like Olanzapine suggest a counter-intuitive possibility: the mechanism might involve a different system entirely.
Researchers theorize that for some of these medications, the effect may be caused by their interaction with the serotonergic system. Specifically, the way these drugs block certain serotonin receptors (known as 5HT2A receptors) could be responsible for inducing compulsive behaviors.
This finding deepens our scientific understanding of addiction. It demonstrates that the pathways to addictive behavior in the brain are incredibly complex and varied, and not solely reliant on the dopamine system that has long dominated the conversation.
Conclusion: A Call for Greater Awareness of Drugs Side Effects
This research serves as a powerful reminder that our understanding of medication side effects is constantly evolving. What is considered safe today may reveal hidden complexities tomorrow. Ongoing research and diligent reporting by healthcare professionals are essential tools for ensuring patient safety long after a drug has been approved.
The study’s findings highlight a potential blind spot in patient care. Life-altering behavioral changes might be mistakenly attributed to personal failings rather than a medication’s side effect.
This leads to a vital question for all of us: Knowing that these risks can go unlisted, how can we foster better conversations between patients and doctors about unexpected changes in behavior?

Do you feel your sexual behavior, or that of someone you love, is out of control? Consult with a professional.
Are you exploring your trauma? Do you feel your childhood experiences were detrimental to your current mental or physical health? Utilize this free, validated, self-report questionnaire to find out.


Are you looking for more reputable data-backed information on sexual addiction? The Mitigation Aide Research Archive is an excellent source for executive summaries of research studies.
