4 Surprising Ways Cannabis Use Disorder Impacts the Brain
More Than a Buzz, According to a Major New Study
As cannabis continues to be legalized for recreational and medical use across North America, public debate often centers on its benefits, risks, and social implications. This has become a public health priority. It’s sparking discussions about everything from tax revenue to addiction potential. Lost in the noise, however, is a more nuanced and critical question: what are the lasting, residual effects on the brain not just from using cannabis, but from developing a Cannabis Use Disorder (CUD)?
For years, research has been muddled by controversy. Some studies suggest significant cognitive decline. Others finding only minimal effects.
A major reason for this confusion is many studies lump together recreational users with those who have a clinical disorder. A new, large-scale meta-analysis published in the journal Addictive Behaviors cuts through this ambiguity by focusing specifically on individuals diagnosed with CUD.
This article distills the four most important takeaways from this major review. Here’s some clear, evidence-based answers on how Cannabis Use Disorder leaves a measurable mark on our cognitive abilities.
1. Cannabis Use Disorder Isn’t Just a Label—It’s a Critical Distinction
Much of the confusion around cannabis’s long-term cognitive effects comes from studies that don’t distinguish between recreational use and a clinical disorder. This new meta-analysis makes that distinction its central focus, and the results are revealing.
The core finding is that while recreational use may be associated with minimal or small deficits, Cannabis Use Disorder is linked to clear, moderate cognitive impairments.
The researchers draw a parallel to alcohol consumption. The cognitive impact seen in individuals with alcohol use disorder is significantly larger than what is observed in those who drink recreationally.
This distinction is the key that unlocks the rest of the study’s findings. Now that we’ve isolated the CUD population, the next question is: what exactly does this impairment look like?
Do you have enough hours for your LPC renewal? Are you in need of continuing education, but bored with the current offerings? Check out Dr. Weeks’ course on Cannabis Use Disorder, and other unique courses on her practice website.
Sexual Addiction Treatment Services has been approved by NBCC as an Approved Continuing Education Provider, ACEP No. 7250. Programs that do not qualify for NBCC credit are clearly identified. Sexual Addiction Treatment Services is solely responsible for all aspects of the programs.
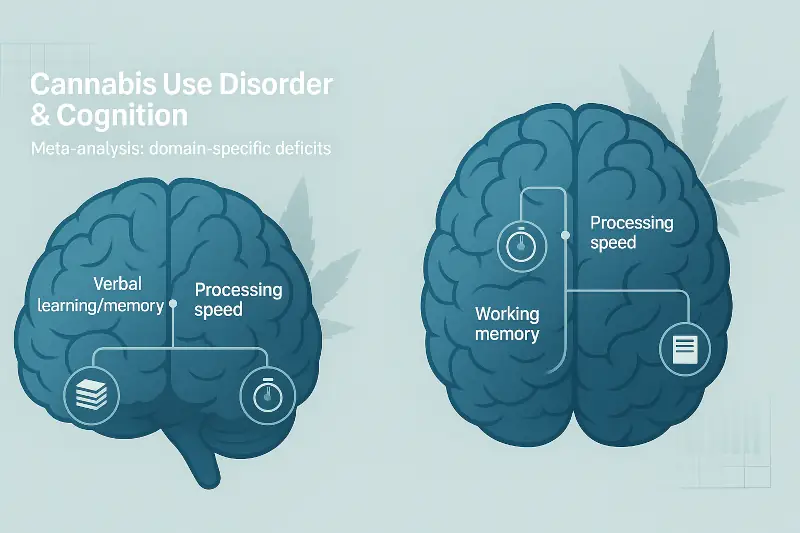
2. The Damage Is Specific, Not Widespread
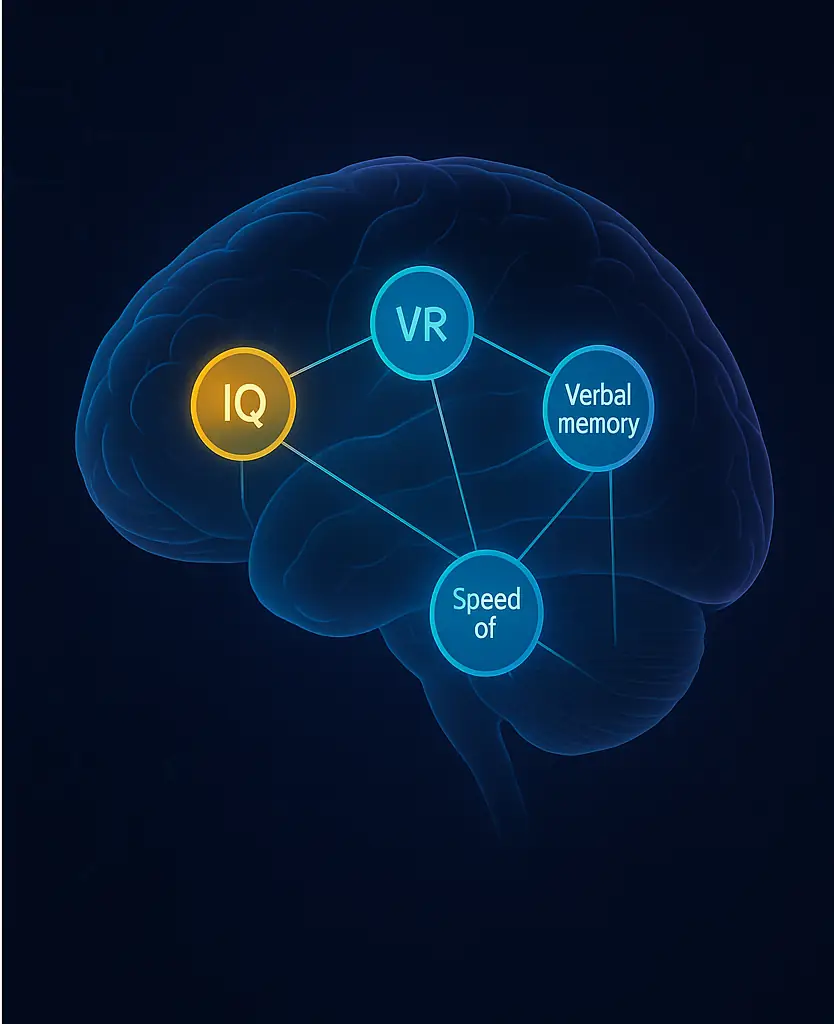
The cognitive impact of CUD isn’t a blunt, uniform fog across the entire brain. Instead, the meta-analysis shows that the impairments are concentrated in specific domains. The study found “small-to-moderate” impairments across several areas, with the largest deficits observed in five key domains:
- IQ: The most significant deficit found. It reflects a moderate impairment in overall cognitive reasoning and problem-solving abilities.
- Verbal Learning: The ability to learn and absorb new information presented through words. It manifests as an impairment making it harder to retain material from a lecture or meeting.
- Verbal Memory: The capacity to recall that learned verbal information later. A deficit can manifest as struggling to remember conversations or key details from something you’ve read.
- Working Memory: The mental “scratchpad” used for holding and manipulating information for short-term tasks. Impairment here makes it harder to follow multi-step instructions or perform mental calculations.
- Speed of Processing: How quickly you can perceive, process, and respond to information. A deficit can slow down reaction times and the ability to keep up in fast-paced conversations or environments.
To emphasize this specificity, the study also identified the cognitive domains that were least affected.
Among them were attention and verbal fluency; the ability to retrieve words from your mind. This targeted impact suggests a more complex mechanism than simple, widespread damage.
3. The Impact of Cannabis Use Disorder Is Comparable to “Harder” Drugs
In a finding that challenges longstanding public perception, the study reveals how the cognitive deficits from CUD stack up against those from other substance use disorders.
The research shows that the magnitude of the impairments in verbal memory and working memory for individuals with CUD is in a similar range to the deficits seen in people with alcohol, cocaine, and methamphetamine use disorders.
However, a critical distinction adds another layer of complexity.
One important difference is that CUD is associated with less diffuse cognitive deficits. While the depth of impairment in those specific memory-related areas is comparable to other substance use disorders, the overall breadth of cognitive damage appears to be narrower.
This directly challenges the common perception of cannabis as a relatively benign substance. Especially when its use escalates to the level of a disorder. The researchers highlight the importance of this finding for how the scientific and medical communities view the substance.
“The similitude of findings between substances confirms the importance of paying attention to individuals with a CUD when studying the residual cognitive effects of cannabis.”
Are you exploring your trauma? Do you feel your childhood experiences were detrimental to your current mental or physical health? Utilize this free, validated, self-report questionnaire to find out.

4. It Presents a Surprising Scientific Mystery
The targeted nature of these cognitive deficits presents a fascinating paradox for neuroscientists.
The primary psychoactive compound in cannabis, Δ9-THC, acts on the brain’s CB1 receptors. From a biological standpoint, this is significant because, as the paper notes, CB1 receptors are “among the most abundant throughout the brain.”
Based on that fact, scientists would expect that chronic, heavy cannabis use would cause diffuse, widespread cognitive effects across many domains.
Yet, as this meta-analysis confirms, the effects are actually quite specific.
This discrepancy suggests the full story is more complex than we currently understand. The authors propose this paradox “indirectly suggests that other cannabinoid receptors than CB1 receptors are mediating the cognitive effects of cannabis,” pointing toward an important new direction for future research.
Conclusion: A Sobering Reminder in the Age of Legalization
This comprehensive meta-analysis sends a clear message: Cannabis Use Disorder is not a trivial condition.
It is linked to real, measurable, and moderate cognitive deficits in crucial areas like memory, processing speed, and overall IQ.
Furthermore, these deficits are not insignificant when compared to those associated with other well-known substance use disorders.
The study’s authors point to a pressing public health concern, noting that “the perceived risk associated with regular cannabis use has been declining in youths since the legalization of the substance.”
While the policy debates will surely continue, this research provides a sobering reminder that the conversation must include a clear-eyed view of the consequences that arise when use crosses the line into a disorder.
As the perception of risk declines, the critical public health challenge becomes clear: how do we effectively communicate the line between casual use and the measurable cognitive costs of a disorder?

Are you a professional looking to stay up-to-date with the latest information on, sex addiction, trauma, and mental health news and research? Or maybe you’re looking for continuing education courses? Then you should stay up-to-date with all of Dr. Jen’s work through her practice’s newsletter!
Are you looking for more reputable, data-backed information on sexual addiction? The Mitigation Aide Research Archive is an excellent source for executive summaries of research studies.

